Learn About Some of the Common Sleep Disorders
At least 40 million Americans each year suffer from chronic, long-term sleep disorders each year, and an additional 20 million experience occasional sleeping problems. These disorders and the resulting sleep deprivation interfere with work, driving, and social activities. They also account for an estimated $16 billion in medical costs each year, while the indirect costs due to lost productivity and other factors are probably much greater. Doctors have described more than 70 sleep disorders, most of which can be managed effectively once they are correctly diagnosed. The most common sleep disorders include insomnia, sleep apnea, restless legs syndrome, and narcolepsy.
Sleep Apnea
Sleep Apnea often goes undiagnosed. Doctors usually can't detect the condition during routine office visits. Also, there are no blood tests for the condition.
Most people who have Sleep Apnea don't know they have it because it only occurs during sleep. A family member and/or bed partner may first notice the signs of Sleep Apnea.
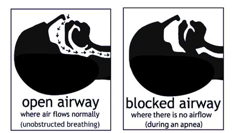
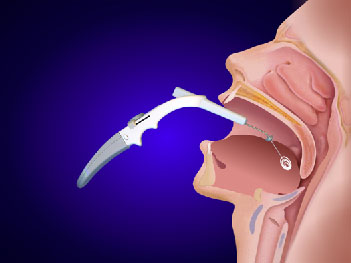
The most common type of Sleep Apnea is obstructive Sleep Apnea. This most often means that the airway has collapsed or is blocked during sleep. The blockage may cause shallow breathing or breathing pauses.
When you try to breathe, any air that squeezes past the blockage can cause loud snoring. Obstructive Sleep Apnea happens more often in people who are overweight, but it can affect anyone.
Types & Definitions
Sleep Apnea (AP-ne-ah) is a common disorder in which you have one or more pauses in breathing or shallow breaths while you sleep.
Obstructive Sleep Apnea (OSA) is a very serious medical disorder caused by repeated blockage of the airway, leading to disruptive sleep and substantial negative fluctuations in blood oxygen levels.
Symptoms of Sleep Apnea include:
Treatment options include:
Consequences of untreated sleep apnea include death, hypertension, stroke, and heart disease. There is also a link to increased risk of industrial and auto accidents primarily due to excessive sleepiness.
[Graphic courtesy of the American Sleep Apnea Association]
Central Sleep Apnea is a less common type of sleep apnea. This disorder happens if the area of your brain that controls your breathing doesn't send the correct signals to your breathing muscles. As a result, you'll make no effort to breathe for brief periods.
Diagnosis - Sleep Testing
Comprehensive sleep testing is often referred to as polysomnography.
The polysomnogram measures multiple bio-signals at the same time while you sleep. These signals include:
The data is collected during an overnight stay at one of the hotel-like bedrooms located at a Sleep & Wellness Sleep Center.
Data is analyzed by credentialed clinicians, with an interpretation and treatment suggestions provided by Board Certified sleep specialist physicians.
In some cases, patients who are certain they do not have other complicating medical conditions or other potential causes of excessive daytime sleepiness (that could ruled out with a comprehensive sleep test), attenuated parameter sleep studies can be done at home.
Contact your local Sleep & Wellness Center for more information.
Sleep Apnea testing
Comprehensive sleep testing is often referred to as polysomnography.
The polysomnogram measures multiple bio-signals at the same time while you sleep. These signals include:
The data is collected during an overnight stay at one of the hotel-like bedrooms located at a Sleep & Wellness Sleep Center.
Data is analyzed by credentialed clinicians, with an interpretation and treatment suggestions provided by Board Certified sleep specialist physicians.
In some cases, patients who are certain they do not have other complicating medical conditions or other potential causes of excessive daytime sleepiness (that could ruled out with a comprehensive sleep test), attenuated parameter sleep studies can be done at home. Contact your local Sleep & Wellness Center for more information.
Treatment Options
PAP (Positive Airway Pressure) Devices:
CPAP: Continuous Positive Airway Pressure. A CPAP device mechanically delivers a preset amount of air pressure through a mask which functions to maintain an open airway during sleep. This pressure eliminates snoring and apnea events.
BiLevel: A PAP device that delivers a higher preset PAP pressure while breathing in (inspiration), and a lower pressure while breathing out. This can make use of a PAP device significantly more comfortable.
Auto-PAP: This type of PAP device can sense apnea events and automatically adjust the amount of air pressure delivered to eliminate apneas while being used, helping to ensure effective (therapeutic) pressures are delivered.
ASV: The Adaptive Servo-Ventilator is a highly complex device that adjusts multiple pressure delivery and breathing rate scenarios to treat patients with Cheyne-Stokes Respiration and Complex Sleep Disordered Breathing (CSDB).

Oral Appliances
These devices are fitted in the mouth and gently press the lower jaw forward, helping pull tissue off the back of the airway reducing apneas when used for appropriate patient populations.
Surgical Procedures
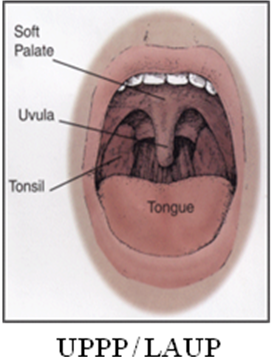
UPPP: Uvulopalatopharyngoplasty. A surgical procedure on the palate in the back of the throat to improve airflow and reduce apnea risk for select patient populations.
LAUP: Laser Assisted Uvulopalatopharyngoplasty. Similar to the UPPP but performed with a laser surgical tool.
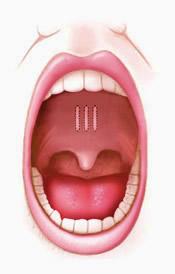
Pillar Implants: A procedure where three small implants are inserted into the back of the throat to stiffen the soft palate to help stop snoring. In some cases, it can also help reduce apneas.
Somnoplasty: This procedure uses Radio Frequency Ablation(RFA) to stiffen tissues in the back of the throat to reduce snoring and apneas in appropriate patients.
Therapy
Oral Appliances
Sleep and Wellness Centers has created a service affiliation with Golden Slumber, Inc., to offer Oral Appliance Therapy as an alternate or adjunctive therapy to CPAP.
Under this program, Sleep and Wellness Centers will perform diagnostic testing on patients referred for suspicion of Obstructive Sleep Apnea. Patients with appropriate clinical indicators and individual preferences will be referred to a local dentist to be fitted for an Oral Appliance.
Golden Slumber is a dentistry-driven company focused on building a network of dentists to provide Oral Appliances for patients referred through this unique arrangement between the local Sleep Center and community dentist. Golden Slumber will train and certify the community dentist on patient application and management of the Oral Appliance. Network dentists will be supplied the Oral Appliance itself (Durable Medical Equipment), and Golden Slumber will manage patient billing and reimbursement; and pay the network dentist a fee for their services.
For more information, Contact Sleep and Wellness Centers at (800) 657-1920.
Narcolepsy
Causes, Incidence and Risk Factors
Narcolepsy (NAR-ko-lep-see) is a disorder that causes a person to have difficulty staying awake. Narcolepsy can cause a person to suddenly fall asleep during the day. These "sleep attacks" occur even after getting enough sleep at night. The unusual and unpredictable sleep pattern that people with narcolepsy have can affect their schooling, work, and social life.
The symptoms of narcolepsy can appear all at once, or they can develop slowly over many years. The four most common symptoms are: excessive daytime sleepiness, cataplexy, which is a sudden, brief loss of muscle control triggered by stress or strong emotion, sleep paralysis, and hypnagogic hallucinations, which are vivid, dream-like experiences that are difficult to distinguish from reality and occur at sleep onset or after awakening.
Narcolepsy is usually diagnosed by a medical history and an overnight sleep study. The next day following a sleep study, a multiple sleep latency test will also be done to determine daytime sleepiness.
Narcolepsy cannot be cured, but its symptoms can usually be controlled so that a person with narcolepsy can lead a normal life. Each treatment plan usually involves medication, life-style changes, and education.
Narcolepsy is a sleep disorder that causes excessive sleepiness and frequent daytime sleep attacks.
Narcolepsy is a nervous system disorder. The exact cause is known.
In some patients, narcolepsy is linked to reduced amounts of a protein called hypocretin, which is made in the brain. What causes the brain to produce less of this protein is unclear.
There is a possibility that narcolepsy is an autoimmune disorder. An autoimmune disorder is when the body's immune system mistakenly attacks healthy tissue.
Narcolepsy tends to run in families. Certain genes are linked to narcolepsy.
Symptoms
Narcolepsy systems usually first occur during ages 15 to 30.
The most common symptoms are:
Signs & Tests
The doctor will perform a physical exam and order blood work to rule out conditions that can cause similar symptoms. Conditions that can cause excessive sleepiness include:
The doctor will perform a physical exam and order blood work to rule out conditions that can cause similar symptoms. Conditions that can cause excessive sleepiness include:
Other tests may include:
Treatment
There is no known cure for narcolepsy. The goal of treatment is to control symptoms.
Lifestyle changes and emotional counseling may help you do better in work and social activities. This involves:
You may need to take prescription medications to help you stay awake. The stimulant drug armodafinil is usually tried first. It is much less likely to be abused than other stimulants. Other stimulants include dextroamphetamine (Dexedrine, DextroStat) and methylphenidate (Ritalin).
Antidepressant medications can help reduce episodes of cataplexy, sleep paralysis, and hallucinations. Antidepressants include:
If you have narcolepsy, you may have driving restrictions. Restrictions vary from state to state.
Expectations
Narcolepsy is lifelong (chronic) condition.
It is not deadly, but it may be dangerous if episodes occur during driving, operating machinery, or similar activities.
Narcolepsy can usually be controlled with treatment. Treating other underlying sleep disorders can improve symptoms of narcolepsy.
Complications
Calling your health care provider
Call your health care provider if:
Source: National Library of Medicine
Insomnia
Causes, Incidence and Risk Factors
Insomniacs have problems either falling asleep or staying asleep. Specifically, they can exhibit: delayed sleep onset, frequent, prolonged arousals during the night, early morning awakenings or low quality sleep.
Most people have experienced insomnia during temporary periods of stress in their life. This is termed acute or short-term insomnia and is usually resolved on its own. However, if the problem persists for more than four weeks, professional advice should be sought.
Are There Different Types of Insomnia? An individual can exhibit either primary or secondary insomnia. Primary insomnia is typically associated with stress and is not associated with other mental or medical problems. Secondary insomnia is the result of underlying problems such as anxiety, mood disorders or medical conditions such as restless legs syndrome or sleep apnea.
Insomnia is trouble falling asleep or staying asleep through the night.
Episodes may come and go (episodic), last up to 3 weeks (short-term), or be long-lasting (chronic).
Sleep habits we learned as children may affect our sleep behaviors as adults. When we repeat these behaviors over many years, they become habits.
Poor sleep or lifestyle habits that may cause insomnia or make it worse:
The use of some medications and drugs may also affect sleep:
Physical, social, and mental health issues can affect sleep patterns, including:
Symptoms
The most common complaints or symptoms in people with insomnia are:
Signs & Tests
Your health care provider will do a physical exam and ask you questions about your current medications, drug use, and medical history. Usually, these are the only methods needed to diagnose insomnia.
Polysomnography, an overnight sleep study, can help rule out other types of sleep disorders (such as sleep apnea).
Treatment
It is important to remember that not getting 8 hours of sleep every night does not mean you are putting your health at risk. Different people have different sleep needs. Some people do fine on 6 hours of sleep a night. Others only do well if they get 10 to 11 hours of sleep.
Treatment often begins by reviewing any drugs or medical conditions that may be causing your insomnia or making it worse.
Thinking about any lifestyle and sleep habits that may be affecting your sleep is an important next step. This is called sleep hygiene. Making some changes in your sleep habits may improve or solve your insomnia.
Using medicine to treat insomnia can sometimes be useful, but there can be risks.
Antihistamines (the main ingredient in over-the-counter sleeping pills) may cause memory problems over time, especially in the elderly.
Only use sedatives under the close care of a doctor, because they can cause tolerance and sometimes dependence. Stopping these medications suddenly can cause rebound insomnia and withdrawal.
Lower doses of certain antidepressant medicines may help. These medicines do not carry the same problems with tolerance and dependence as sedatives.
It may help to see a psychiatrist or other mental health provider to test for a mood or anxiety disorder that can cause insomnia.
They may use talk therapy, such as cognitive-behavioral therapy, to help you gain control over anxiety or depression.
A psychiatrist may also prescribe antidepressants or another medicine to help your sleeping problem and any mood or anxiety disorder you might have.
Expectations
Expectations (prognosis)
Most people are able to sleep by practicing good sleep hygiene. See a doctor if you have insomnia that does not improve.
Complications
Daytime sleepiness is the most common complication of insomnia. There is also evidence that a lack of sleep can lower your immune system's ability to fight infections.
A lack of sleep is also a common cause of auto accidents. If you are driving and feel sleepy, take a break.
Calling your health care provider
Call your doctor if insomnia has become a problem.
Source: National Library of Medicine
Restless Legs Syndrome
Causes, Incidence, and Risk Factors
Restless leg syndrome is a disorder in which there is an urge or need to move the legs to stop unpleasant sensations.
Restless leg syndrome (RLS) occurs most often in middle-aged and older adults. Stress makes it worse. The cause is not known in most patients.
RLS may occur more often in patients with:
RLS is commonly passed down in families. This may be a factor when symptoms start at a younger age. The abnormal gene has not yet been identified.
Restless leg syndrome can result in a decreased quality of sleep (insomnia). This lack of sleep can lead to daytime sleepiness, anxiety or depression, and confusion or slowed thought processes.
Symptoms
RLS leads to sensations in the lower legs between the knee and ankle. The feeling makes you uncomfortable unless you move your legs. These sensations:
Most patients have rhythmic leg movements during sleep hours, called periodic limb movement disorder (PLMD).
All of these symptoms often disturb sleep. Symptoms can make it difficult to sit during air or car travel, or through classes or meetings.
Symptoms may be worse during stress or emotional upset.
Signs & Tests
There is no specific test for restless leg syndrome.
The health care provider will not usually find any problems, unless you also have peripheral nerve disease.
Tests will be done to rule out disorders with similar symptoms, including iron deficiency anemia.
Treatment
There is no known cure for restless leg syndrome.
Treatment is aimed at reducing stress and helping the muscles relax. The following techniques may help:
Low doses of pramipexole (Mirapex) or ropinirole (Requip) can be very effective at controlling symptoms in some people.
If your sleep is severely disrupted, your health care provider may prescribe medications such as Sinemet (an anti-Parkinson's medication), gabapentin and pregabalin, or tranquilizers such as clonazepam. However, these medications may cause daytime sleepiness.
Patients with iron deficiency should receive iron supplements.
Low doses of narcotics may sometimes relieve symptoms of restless leg syndrome.
Expectations
Restless leg syndrome is not dangerous or life-threatening, and it is not a sign of a serious disorder. However, it can be uncomfortable and disrupt your sleep, which can affect your quality of life.
Complications
Insomnia may occur.
Calling your health care provider
Call for an appointment with your health care provider if:
Prevention
Techniques to promote muscle relaxation and stress reduction may reduce the incidence of restless leg syndrome in people prone to the condition.
Source: National Library of Medicine